SOAP notes have grow to be indispensable frameworks guiding medical documentation throughout healthcare. This text gives psychological well being professionals with an in-depth information on leveraging SOAP notes to reinforce affected person care by correct record-keeping.
Gathering Subjective Knowledge Important in Psychological Well being
The ‘S’ in SOAP notes stands for subjective information, a essential part in psychological well being, the place almost 50% of diagnoses are derived from patient-reported signs (Nationwide Institute of Psychological Well being).
Constructing belief and rapport facilitates disclosures, that are integral to assessments and remedy plans. Take into account dialog starters and instruments like journals, surveys, apps, and scales. Doc particulars utilizing the shopper’s personal phrases whereas avoiding assumptions or interpretations.
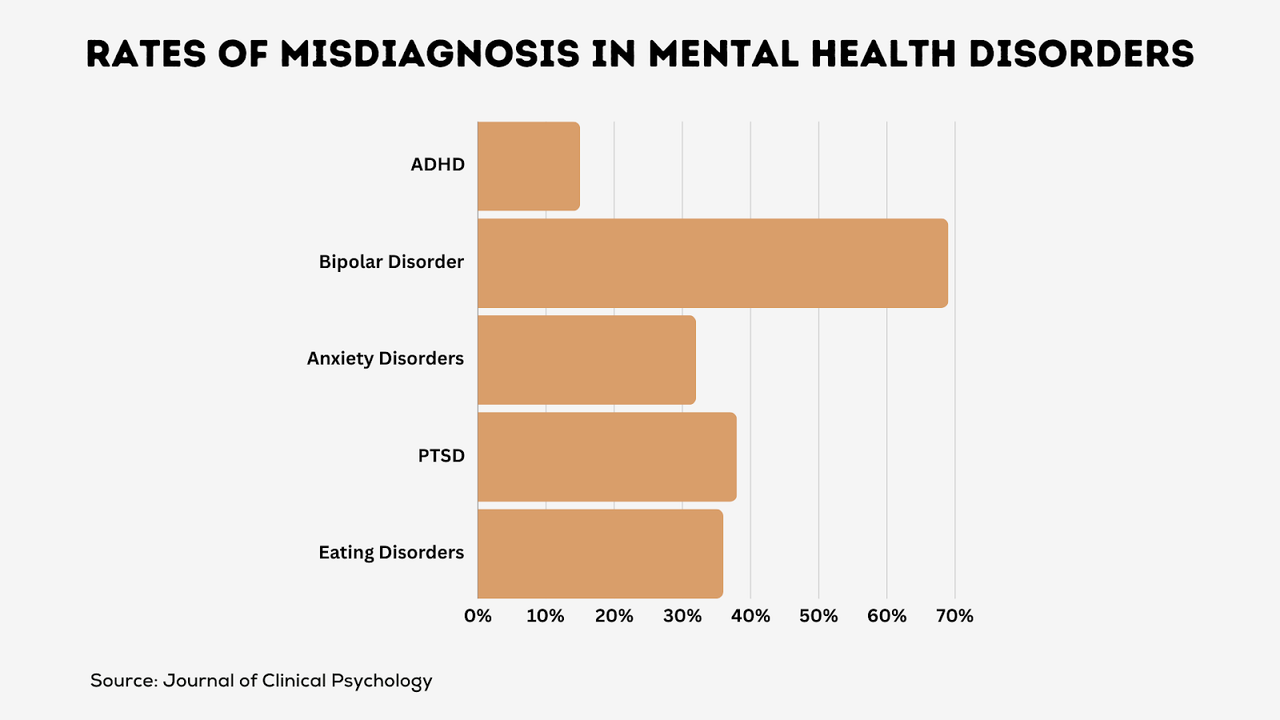
Correct symptom seize additionally prevents misdiagnoses carrying dangers of inappropriate remedy. For instance, signs like distraction, widespread to each anxiousness and ADHD, may point out both situation with out adequate subjective information detailing the affected person’s expertise. Affected person privateness stays paramount when dealing with delicate private data.
> Sturdy therapeutic alliances and high quality subjective information assortment related to higher psychological well being outcomes. (Psychiatric Companies)
Infusing Objectivity Into Psychological Well being Documentation
The “O” part information goal observations together with:
- Look, orientation, temper, have an effect on, speech patterns, thought processes
- Findings from diagnostic exams, structured interviews, validated ranking scales
- Behavioral modifications over time primarily based on longitudinal information
Standardized instruments like PHQ-9 melancholy scales, anxiousness inventories, suicide danger assessments, and trauma checklists assist quantify signs.
> Goal metrics set up baselines for monitoring psychological well being progress. (Psychological Evaluation)
These instruments additionally assist counteract subjective biases that might affect assessments. Formal diagnoses ought to align with DSM standards, incorporating structured evaluations that reveal ranges of performance.
Making Knowledgeable Assessments in Psychological Well being Settings
Subsequent, the “A” paperwork insights into diagnoses, underlying mechanisms, and readiness for change. Assessments combine:
- Shopper background, medical historical past, and prior information
- Diagnoses differentials – rule out prospects
- Bio-psycho-social formulations figuring out causal and sustaining components
For instance, anxiousness associated to the current lack of a job and marital points might hyperlink biology (genetic predisposition) with circumstantial stressors and protecting components like social help.
> Correct prognosis is important – misalignment typically results in poor psychological well being outcomes. (World Psychiatry)
Crafting Personalised Care Plans in Psychological Well being
The ‘P’ in SOAP notes refers to remedy plans that tackle areas in want of intervention. Good plans outline:
- Objectives – What ought to enhance? Desired outcomes?
- Targets – Incremental steps towards objectives
- Interventions – Therapies, methods, and applications to deploy
- Progress metrics – Symptom ranking scales, surveys, behavioral analyses
- Observe-ups – Plan adjusts primarily based on measurable change
Collaborative goal-setting that respects shopper priorities is important. For instance, a depressed younger grownup might want to:
- Objective: Resume school in 6 months
- Goal: Attend 3 lessons subsequent semester whereas elevating temper ranking from PHQ-9 rating of 15 to beneath 10
- Interventions: Cognitive behavioral remedy, anti-depressant remedy, month-to-month supplier follow-ups
- Metrics: PHQ-9 scale, semester course load monitoring
Finest Practices for Psychological Well being Documentation
Psychological well being employees doc their sufferers’ progress utilizing SOAP notes. For these new to this observe, trying into SOAP Notice examples can considerably improve the effectiveness of recording important data. Given the private and personal nature of those notes, healthcare employees should train utmost care to make sure they’re written precisely and helpfully. Listed here are 5 ideas:
1. Write a Detailed Private Story
Share the total image from classes with out guessing causes. Merely state what you see and listen to. For instance:
- Todd seemed drained with saggy eyes
- Alicia cried for quarter-hour speaking about her mother
- Jose mentioned he feels frightened in school
Each little element issues when attempting to assist.
2. Maintain notes personal and safe
Well being data is personal! Observe all ethics guidelines on:
- Locking up notes
- Needing affected person consent to share
- Utilizing on-line instruments safely
Clarify to sufferers the way you defend their privateness. Additionally share if others generally might even see notes, like if a physician consults. Guarantee sufferers they’ll decide out.
3. Set up notes rigorously
Construction helps! Group-related observe elements. Checklist signs collectively. Use traces or headings. Write session highlights on the prime. Put them in time order. This makes lengthy notes simpler to scan later.
4. Write notes ASAP
Particulars fade quick! Jot session notes down alongside the way in which or proper after whereas it’s contemporary. This ensures you seize and share key bits finest.
5. Evaluation with sufferers
Make clear with sufferers that notes intention to assist. Examine on the finish of classes:
- Did I miss or misunderstand something?
- Do you see the progress we’re making?
- What subsequent step appears smartest?
Partnership results in higher care!
Bear in mind, cautious progress notes information higher psychological well being care. Practice arduous in writing useful SOAP notes.SMALL every day good points make BIG modifications over time!
Integrating SOAP Notes into Psychological Well being Follow
SOAP notes considerably improve the supply of psychological well being providers by:
- Selling continuity and coordinated care plans throughout multidisciplinary groups
- Permitting measurement of intervention effectiveness per progress rankings
- Capturing complete information trails on the diagnostic and remedy trajectories
- Producing customizable standing summaries for shopper communication
- Defending authorized pursuits in case of lawsuits by detailed documentation
Continuously Requested Questions
What ethics or guidelines ought to healthcare employees comply with with progress notes?
Earlier than beginning notes, get hold of the affected person’s consent and clearly clarify how their private data may be shared. Make certain sufferers can decide out of sure issues at any time when they need.
How can SOAP notes help totally different healthcare employees in collaborating to help the affected person?
SOAP notes comply with the identical construction throughout all specialties. So that they make it simpler for medical doctors, counselors, nurses, and others to grasp a affected person’s scenario when working collectively or handing off care.
What are some laptop applications that help with creating and managing progress notes?
Sure! Good digital instruments could make SOAP notes simpler and sooner to place collectively, share with different care suppliers, analyze to seek out tendencies, and enhance over time. Some in style choices used at present are SimplePractice, DrChrono, and NextGen.
Backside Line
In brief, cautious SOAP note-taking results in higher psychological well being diagnoses, smarter subsequent steps, and care that places the affected person first. It additionally lets extra healthcare employees collaborate to help that affected person.
Whereas studying to write down efficient progress notes takes observe, the trouble is worth it. Small good points at present deliver large wins for care sooner or later. Moreover, digital instruments can be found to simplify and improve this course of.









